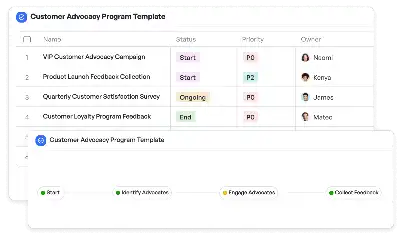
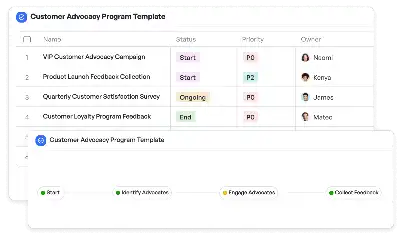
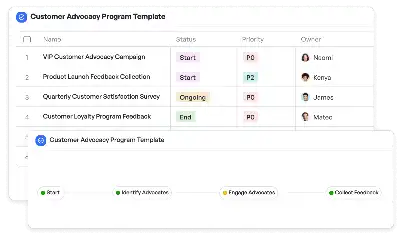
Insurance Prior Authorization Workflow
Achieve project success with the Insurance Prior Authorization Workflow today!
What is Insurance Prior Authorization Workflow?
Insurance Prior Authorization Workflow is a structured process designed to ensure that medical services, procedures, or medications are approved by insurance providers before they are delivered to patients. This workflow is critical in the healthcare industry, where compliance with insurance policies and cost management are paramount. By implementing this workflow, healthcare providers can avoid claim denials, ensure timely patient care, and maintain transparency in the approval process. For example, when a patient requires a high-cost procedure like an MRI scan, the workflow ensures that all necessary documentation and medical justifications are submitted to the insurance company for review and approval. This not only streamlines the process but also minimizes delays in patient treatment.
Try this template now
Who is this Insurance Prior Authorization Workflow Template for?
This Insurance Prior Authorization Workflow Template is ideal for healthcare administrators, insurance coordinators, and medical practitioners who are involved in the pre-approval process for medical services. Typical roles include hospital billing staff, insurance verification specialists, and case managers. For instance, a hospital's insurance coordinator can use this template to track and manage multiple authorization requests simultaneously, ensuring that each request is processed efficiently and in compliance with insurance requirements. Similarly, a private clinic's administrative staff can rely on this workflow to handle prior authorizations for outpatient procedures, reducing the risk of claim rejections.
Try this template now
Why use this Insurance Prior Authorization Workflow?
The Insurance Prior Authorization Workflow addresses specific pain points in the healthcare industry, such as delays in obtaining insurance approvals, lack of standardized processes, and communication gaps between providers and insurers. By using this template, healthcare providers can ensure that all required documentation is submitted accurately and on time, reducing the likelihood of claim denials. For example, the workflow includes steps for verifying patient insurance details, reviewing medical necessity, and obtaining approvals, which are critical for high-cost treatments like chemotherapy or specialized surgeries. Additionally, the template provides a clear framework for tracking the status of each authorization request, enabling healthcare teams to focus on patient care rather than administrative bottlenecks.
Try this template now
Get Started with the Insurance Prior Authorization Workflow
Follow these simple steps to get started with Meegle templates:
1. Click 'Get this Free Template Now' to sign up for Meegle.
2. After signing up, you will be redirected to the Insurance Prior Authorization Workflow. Click 'Use this Template' to create a version of this template in your workspace.
3. Customize the workflow and fields of the template to suit your specific needs.
4. Start using the template and experience the full potential of Meegle!
Try this template now
Free forever for teams up to 20!
The world’s #1 visualized project management tool
Powered by the next gen visual workflow engine




